Reprinted from the spring issue of The Ohio Family Physician
By: Christen Johnson, MD, MPH, Heart of Ohio Family Health Centers
Physician burnout, or the combination of “emotional exhaustion, depersonalization, and a sense of reduced personal accomplishment,”1 has been a concern in the physician community for decades. Once thought to be a product of improved technology and increased demands on physicians, studies report burnout plagued at least 50% of trainees and physicians1,2,3 and its impact reaches much further than decreased productivity. Using the “Conservation of Resources Theory,”2 burnout is a product of increases in utilization of personal resources in response to increasing demands.
Once resources have been depleted, burnout is a natural coping mechanism that, “creates emotional distance”2 to preserve what resources are left. Since February 2020, with the dawn of the COVID-19 pandemic, the global demands on physicians have exponentially increased. Physicians have risen to every call from inadequate personal protective equipment, brand new methods for reaching patients, and record numbers of deaths, to fighting medical misinformation and legalistic concerns that impact patient and physician safety,2,4 but at what cost?
Reports show that physician burnout impacts both patients and physicians through decreases in the quality of care and patient satisfaction, and decreases in physician wellness and mental health that can lead to substance abuse, depression, and suicide.1,2,3,4,5 Further, as studies show that high mortality rates increase emotional exhaustion,1 the impact of the COVID-19 pandemic has increased attending physician burnout rates by 23%-62%, depending on physician location, and 76% among residents.5 Primary care specialties like family medicine are among the most impacted.5 External hobbies and social supports were previously protective factors against burnout, but as closures and the risk of transmitting coronavirus to loved ones remains, many physicians are reporting increases in feelings of isolation, frustration, and continued fear.4 According to some studies, the added stressors associated with the pandemic could even precipitate PTSD for some frontline workers, including physicians, creating staggering impacts on physician mental health for years to come.6
The economic impact of COVID-19 on the global workforce is evident through The Great Resignation – and the field of medicine has been no exception. Physician burnout alone “more than doubled self-reported intent to leave one’s current practice for reasons other than retirement”1 with annual losses equivalent to “the graduating classes of seven medical schools”1 each year. This paired with the added stresses of staffing shortages and unpredictability in being a health care professional during COVID-19 brings forth a daunting reality, especially in the setting of a long-standing physician shortage. There is no way to know just how many physicians we may lose to early retirement and career changes after this.6,7 Worse, more than 100,000 health care workers have died8 while caring for patients during the pandemic globally, including now more than 3,600 Americans as reported in April 2021.9
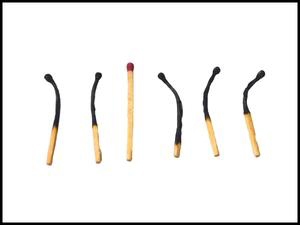
However, in all of this despair, there is hope. As the media has likened physicians to heroes fighting COVID-19, their microscopic foe, the field has united across specialty lines in a spirit of altruism to support one another. While the traditional recommendations including mindfulness programs,1,3,4,5 environments that encourage work-life balance,1,2,3,4,5,6 supportive teams,1,2,3,4,5,6 and individual supports through family, friends, and counselors2,3,4,5 remain key in keeping burnout at bay, medicine will emerge from the COVID-19 pandemic with an opportunity to change the trajectory of the field. For the first time, the stigma surrounding physician-heroes needing to ask for help is beginning to lift. The challenges of these completely mortal heroes are being understood as more than just needing resilience, a resource itself that physicians already have. Rather than “tough[ing] it out,”2 physicians could be walking into a new norm of workplace culture that centers on valuing the physician themselves as a resource, rather than only their productivity.2,4,5 The American Medical Association suggests that COVID-19 has created space to have more conversations leading to healing: conversations about well-being when discussing changes to policies and procedures,10 conversations that empower and acknowledge physicians,10 and conversations that share physician experiences.11 The American Academy of Family Physicians has also created opportunities for physicians to learn how to lead family medicine in this charge.12 Changing how physicians are expected to interact with self, allowing for self-compassion and normalizing the ability to tend to human needs, makes medicine human again. Changing how physicians see themselves changes how they care for themselves, see their profession, and ultimately can improve how they care for their patients. If there is anything that the COVID-19 pandemic has brought, it’s change.
Resources available on the Ohio Academy of Family Physicians website.




